Health sector
Home > Sectors of activity > Health
What are the challenges of hygiene
in the health sector?
Oxy’Pharm was inspired from a desire to invest in the fight against nosocomial infections, and is now present in many healthcare institutions to guarantee perfect hygiene. The proposed solutions are compliant with health protocols imposed by the government. Bionic cleaning and bio-disinfection solutions that have proven their effectiveness against all germs (including resistant germs) over the years. The devices are standardised and easy to use. All of these solutions save valuable time for healthcare staff.
Sanivap,
steam bio-cleaning
To prevent infectious risks in the healthcare sector, it is essential to take into consideration the role played by the environment, in particular surfaces, which can contribute to cross-contamination. In response to this problem, Sanivap devices provide complete bio-cleaning. These devices produce high temperature steam which guarantees their effectiveness in terms of detergent: elimination of dirt and biofilms, no residual chemical traces.
The generators and a wide range of accessories mean that the steam penetrates into the smallest corners to remove dirt, making cleaning easier, more effective and longer lasting.
Nocotech,
automated bio-disinfection
The Nocotech automated bio-disinfection solution is based on the dual action of a treatment device and a disinfectant product. It marks the terminal decontamination and disinfection operation within healthcare facilities. This solution is used for all surfaces, including the most difficult to access ones, to reach the level of microbiological cleanliness that will lead it, later on, to meet the qualification standards for the cleanroom.
A fully biodegradable solution, safe for health and environmentally friendly.
The system can also be used for insecticide or deodorant treatment.
Glosair,
automated bio-disinfection with advanced technology
The Glosair solution is also based on the dual action of an automated surface treatment device and a disinfectant product. The difference is that it is a high-tech solution that makes it easier to control and trace all of the treatments. The Glosair solution therefore allows for high-quality follow-up of users.
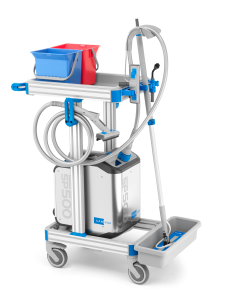
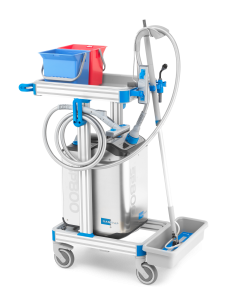
Alpha Clean,
pre-disinfection of instruments
Healthcare institutions are faced with several problems related to medical devices with cavities. To solve this issue, the Alpha Clean range, which consists of a disinfecting auto-washer and a detergent solution, is used to pre-disinfect the instruments. An operation that consists of immersing the instruments in a detergent and disinfectant solution (bactericide) immediately after use. It prevents organic material from settling due to drying, the contamination of workers and the contamination of the environment. As soon as they are no longer in use, it is essential to irrigate the canals in order to remove any dirt immediately.